What is hyponatremia?
Hyponatremia is a decrease in blood plasma sodium (Na) levels below 135 mmol/L. This condition has a wide range of causes, from excessive water intake with an unsalted diet, uncontrolled use of medications to severe kidney disease and malignant tumors. Clinical symptoms are mainly represented by neuropsychiatric disorders (Mephedrone-induced Hyponatremia). Diagnosis is made on the basis of determining the level of sodium and serum osmolarity, urine. Treatment should include control of the cause, administration of isotonic or hypertonic saline solutions, maintenance of euvolemia.
Hyponatremia is the most common electrolyte disorder encountered in clinical practice. Sodium is a vital macronutrient that performs many functions in the human body (providing resting and action potential, maintaining plasma osmotic pressure, acid-base equilibrium). Decreased Na concentration primarily adversely affects neuronal function. The majority of cases of this condition occur in intensive care unit patients (about 15-20%).
The severity of hyponatremia depends on the resulting osmolality or amount of sodium per kg of total body water. In most clinical reports, hyponatremia is an asymptomatic condition, detectable only by biochemical tests in body fluids. In more severe situations, signs and symptoms of hyponatremia develop; they are usually nonspecific and include nausea and vomiting, headache, loss of energy, drowsiness and fatigue, restlessness, irritability, confusion, muscle weakness and spasms or seizures.
Extreme cases can end in serious illness because the primary organ affected is the brain. In such situations, failure to intervene quickly can lead to seizures, coma, herniated cerebellar tonsils, severe neurological damage, and even death.
The severity of hyponatremia is divided into:
- Mild – 130 to 134 mmol/l;
- Moderate – 125 to 129 mmol/l;
- Severe – less than 125 mmol/l.
According to the rate of development of hyponatremia can be:
- Acute – lasting up to 48 hours;
- Chronic – lasting more than 48 hours.
Effect of mephedrone on hyponatremia
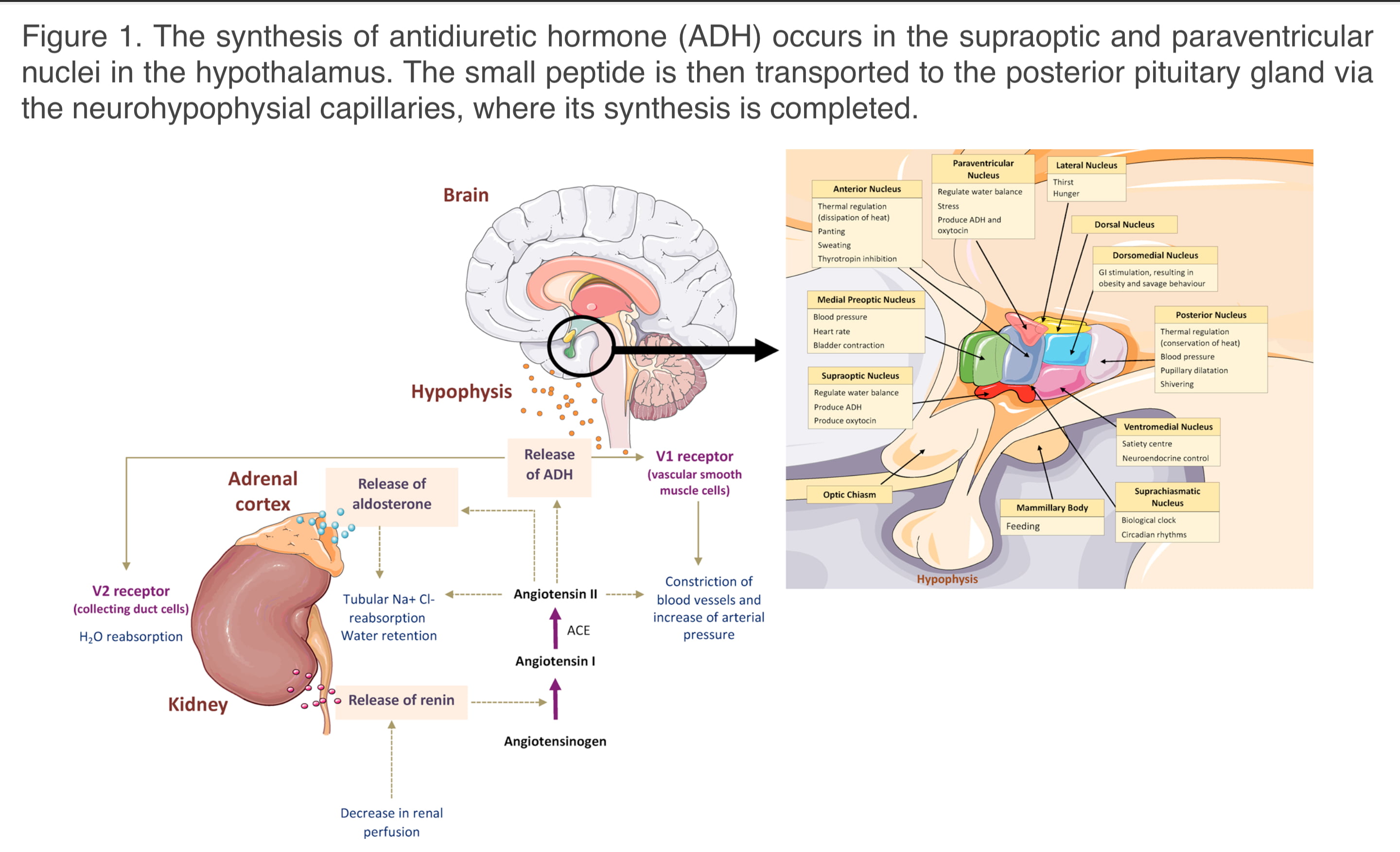
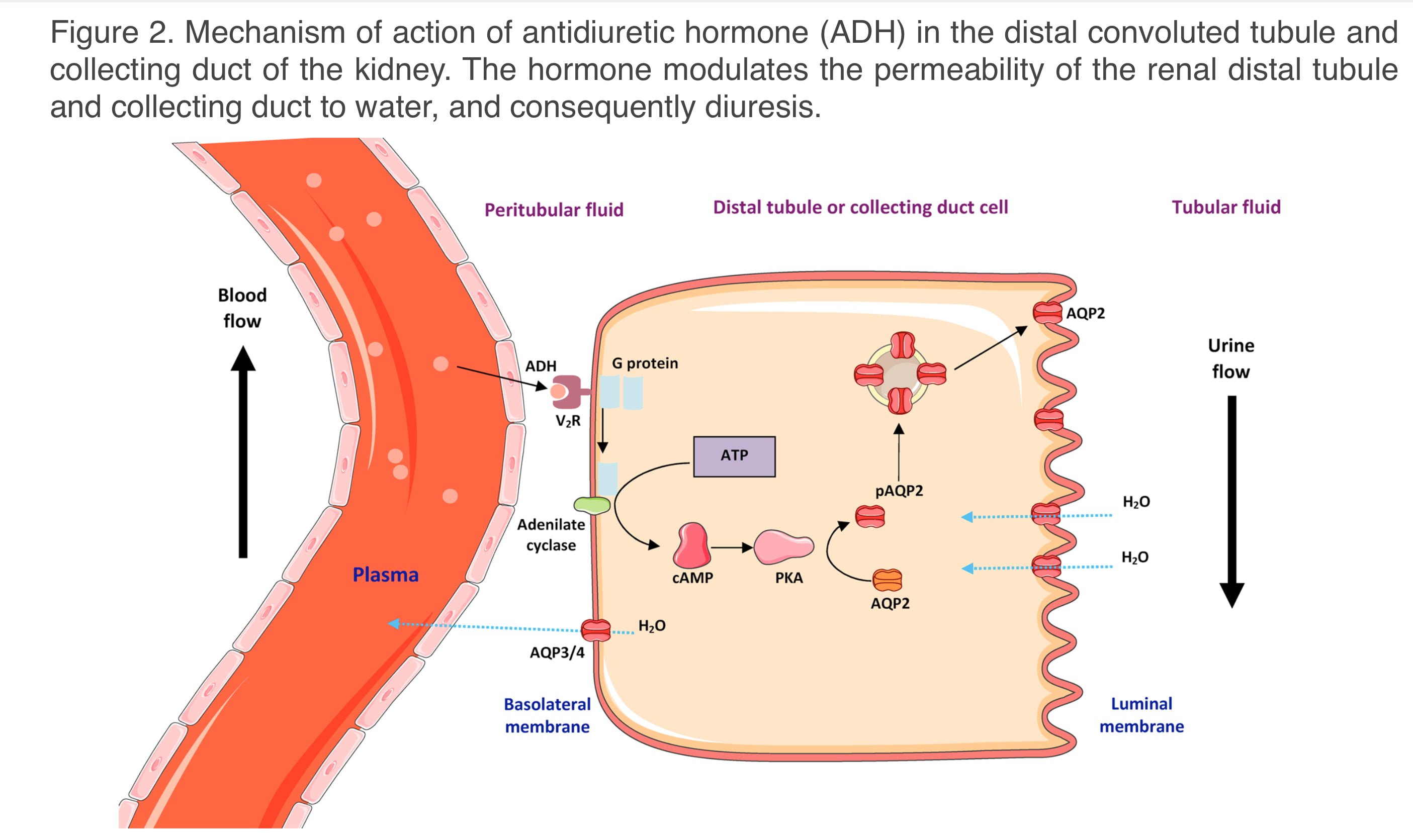
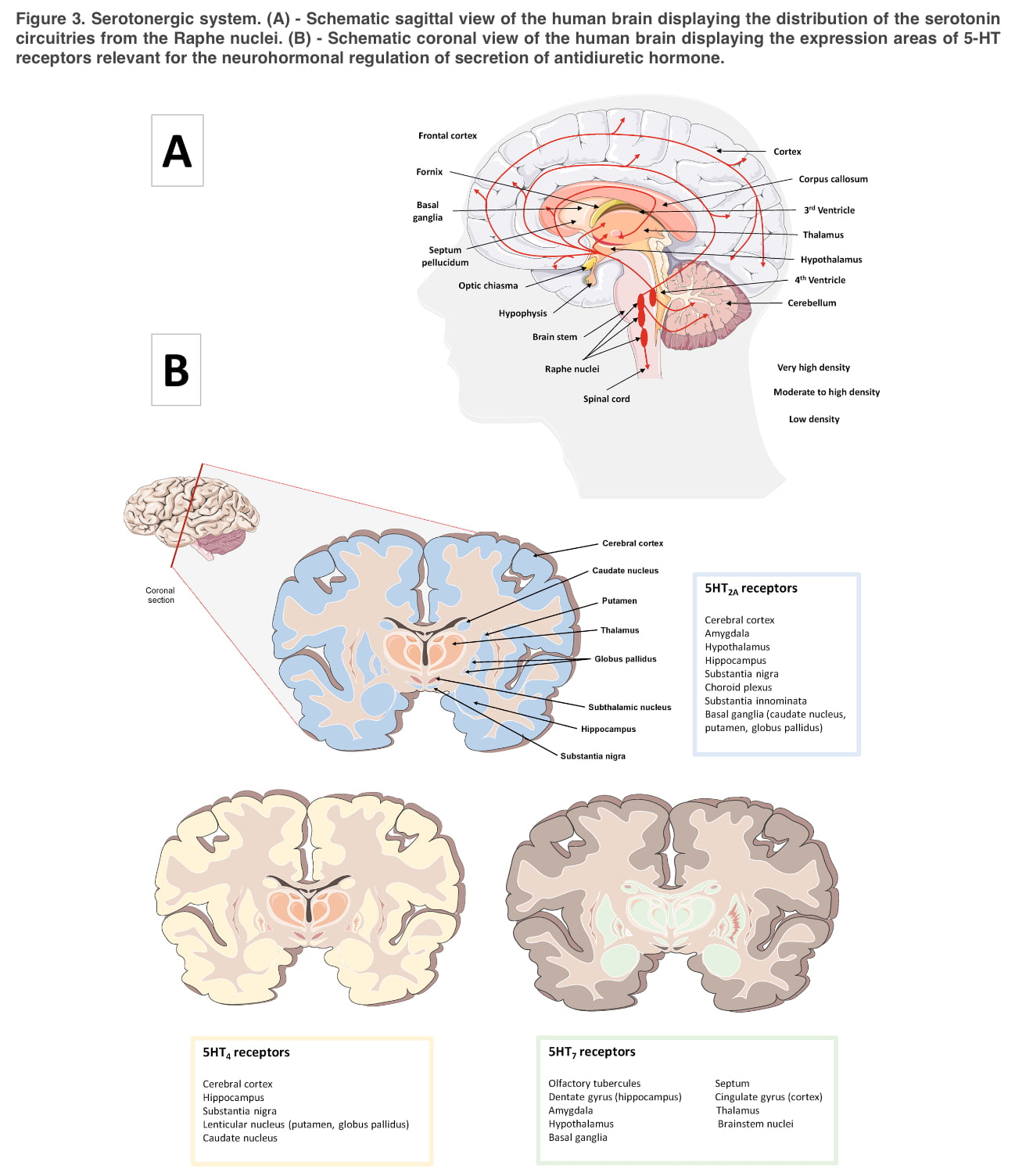
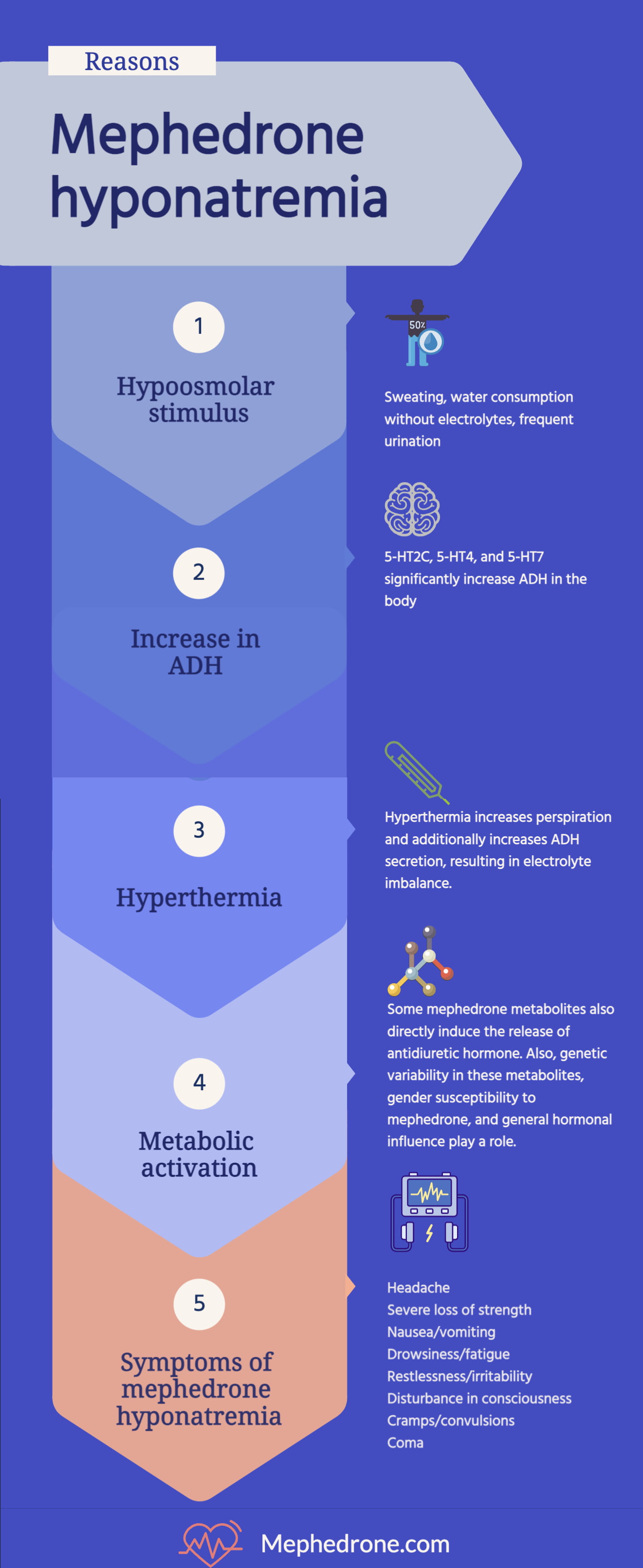
The mechanisms responsible for the development of hyponatremia as a result of mephedrone use, particularly those associated with altered ADH secretion, are not fully understood. However, metabolic activation , genetic variability, serotonergic regulation of neurohormonal secretion, hyperthermia, gender predisposition and hormonal influence are among the most important factors contributing to this disease.
Because the effects of mephedrone result in excessive stimulation of the serotonergic system, and the release of antidiuretic hormone is mediated by 5-NT, one would predict that mephedrone-induced hyponatremia would at least be due to changes in serotonergic regulation of neurohormonal antidiuretic hormone secretion.
In most cases, depending on the severity of mephedrone hyponatremia, the user will experience the following symptoms:
- Headache;
- Severe loss of strength;
- Nausea;
- Vomiting;
- Drowsiness and fatigue;
- Restlessness;
- Irritability;
- Confusion;
- Muscle weakness;
- Spasms/convulsions;
- Coma.
History of mephedrone use in people suffering from hyponatremia
Case report one: a 15-year-old girl developed mental status changes, nausea and vomiting after consuming a white powdery substance along with alcohol the night before. Her Glasgow Coma Scale score was 11, blood pressure 108/58 mmHg, pulse rate 54 per minute, respiratory rate 15 per minute.
Arterial blood gases and electrocardiography were normal. CT scan of the brain showed no features, but cerebrospinal fluid pressure was elevated. There was marked hyponatremia (118 mmol/L); serum osmolality was low (256 mmol/L), but urine osmolality was high (742 mmol/L).
Urinalysis confirmed mephedrone intoxication. Presumptive diagnosis: mephedrone-induced euvolemic hypoosmotic hyponatremia with encephalopathy and increased intracranial pressure. With fluid restriction, her electrolyte imbalance resolved within 24 hours, and she became alert and oriented, with no focal neurologic abnormalities other than mild dysphasia and anterograde amnesia.
Three days after hospitalization, a brain MRI scan showed multifocal abnormalities of subcortical signals. She fully recovered in 3 months.
Case report two: A 22-year-old woman was taken to the Emergency Department after several episodes of tonic-clonic seizures, several hours after ingestion of mephedrone. The patient required intubation due to recurrent seizures and was found to have severe hyponatremia (120 mmol/L), which was treated with hypertonic saline. The patient’s mental status rapidly improved and she was extubated the day after admission.
Prevention of mephedrone-induced hyponatremia
To alleviate the thirst and hyperpyrexia caused by mephedrone use, addicts often consume water (without electrolytes), ethanol, or soft drinks, which increases the risk of edema. Because of the dangers associated with the severe elevated body temperature caused by mephedrone use, it is advisable to avoid taking large amounts of fluids that are devoid of electrolytes. Hypotonic drinks should be avoided and cold isotonic fluids, or sodium chloride-hydrocarbonate sports drinks should be used.
Alcohol and large amounts of caffeine should be avoided, as they can only exacerbate sodium loss due to complex renal function, which affects certain parts of the kidneys (proximal and distal renal tubules, collecting tubes) and also have a suppressive effect on renal synthesis (prostaglandin E2, a potent antidiuretic hormone receptor antagonist).
Hyponatremia is also provoked by profuse sweating, a consequence of both altered thermoregulation and increased activity associated with prolonged dancing. Therefore, it is recommended that users avoid crowded and hot places such as rave and techno parties and nightclubs, and that they consume mephedrone in well-ventilated rooms with good air flow.
In addition, reducing physical exertion caused by intense dancing and/or establishing recovery periods to cool down and lower body temperature is recommended.
First Aid
Given that the diagnosis of mephedrone-induced hyponatremia can be identified solely on clinical assessment of extracellular fluid volume by laboratory parameters (plasma osmolarity, urine osmolarity and sodium concentration), specific care should be provided exclusively in hospital settings. However, the following algorithm of actions should be used as first aid:
- Call an ambulance (in case of impaired consciousness)
- Stop using mephedrone and other psychoactive substances immediately
- Stop all physical activity
- Cool the person down (take a warm shower with a gradual decrease in water temperature/place a wet cold towel on the head)
- Abundant drinking of chloride-hydrocarbonate-sodium water (water should contain a large amount of electrolytes)
- Take 5 mg of prednisolone once
Summary
One of the major consequences of serotonergic deregulation with mephedrone use is altered release of antidiuretic hormone, which can lead to SIADH, a condition potentiated by hyperthermia, excessive water intake, and loss of sodium with sweat. SIADH can end in hyponatremia.
Typically, hyponatremia is associated with hypervolemia. which leads to dilution of plasma sodium and subsequent intracellular water movement. Decreased plasma sodium can provoke changes in mental status and lead to coma, tonic-clonic seizures, cerebral edema, cerebellar amygdala wedging, and cerebral death.
Common therapeutic measures include administration of a hypertonic solution in situations of acute symptomatic hyponatremia with central nervous system involvement, followed by fluid restriction to correct plasma sodium levels. It is particularly important that health care providers treating clinical intoxication be informed about the mechanisms underlying this phenomenon in order to select the most appropriate therapeutic measures.