Back in 2016, the Lancet published an article stating that mephedrone-related deaths are on the rise in many countries, with death rates already nearly comparable to MDMA-related deaths. The strong addictive potential of mephedrone increases the risk of people being hospitalized in the future. According to data published in the journal Lancet Psychiatry, the younger the person, the higher the dose of mephedrone he or she took and the longer the mephedrone binge lasted.
The combination of new psychoactive substances has a negative effect on liver function. To date, there are no publications related to studies of liver enzyme levels involving mephedrone users. Only sporadic publications describe cases of acute liver failure after using synthetic cathinones.
One of the most common infections among users of various drugs is hepatitis C virus. According to statistics in the U.S., the prevalence in the population of active drug users ranges from 60% to 90%. Given that all cathinones (in particular mephedrone) have hepatotoxic effects, the presence of HCV infection in a person increases the risk of developing additional damage to the liver parenchyma several times.
There is no data in the literature on the effects of the consumption of NPSs (including mephedrone) with other psychoactive substances on the incidence of HCV infection. Only a single publication, namely the one from 2019, indicates that there is an increased risk of HCV infection in the group of patients injecting new psychoactive substances. However, this type of data is general and does not include tests focused on individual drugs taken with new psychoactive substances, i.e., their effects on the risk of HCV infection.
A review of the various literature suggests that the NPS combination only blurs the clinical picture. It is often the case that people who use mephedrone actually take a mixture in which the actual amount of mephedrone is negligible and the bulk of the powder consists of toxic impurities that could potentially have hepatotoxic effects.
Given that people who use mephedrone often combine it with other psychoactive substances (including sedative benzodiazepines), one of the main goals of the present study is to find out whether any of these combinations increase the risk of additional liver damage and how likely HCV infection is to occur when different drug combinations are used. Among other things, the goal is to see if there are differences in liver enzyme levels between a group of people who use mephedrone in conjunction with alcohol, heroin, or benzodiazepines (including in the absence of mephedrone). Also, we found out whether there is a significant interaction in the group of people with HCV infection (whether there is an effect on ALT and AST levels).
Design and method of experimentation
This study involved 330 patients who used mephedrone in conjunction with other psychoactive substances. The additional drugs were: alcohol, heroin and benzodiazepines. The comparison group consisted of 180 patients with alcohol addiction and 152 patients with benzodiazepine addiction. To put it in another way, the comparison concerned those not taking mephedrone, but addicted to alcohol, heroin, or benzodiazepines alone.
Alanine transaminase (ALT) and aspartate transaminase (AST) were measured in the compared groups of patients. Anti-HCV antibodies were measured in the six compared groups of patients, namely those addicted to alcohol, heroin, or benzodiazepines, as well as in groups taking mephedrone alongside these psychoactive substances. Genetic material (RNA) of HCV was examined to confirm current infection.
Results and discussion
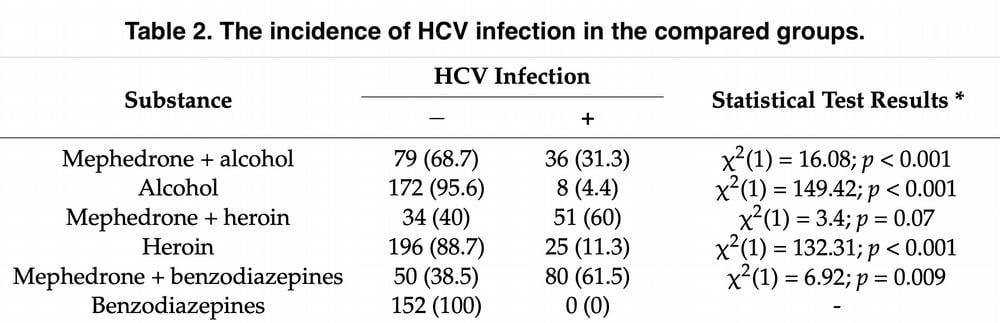
Of the 330 patients, 34.8% combined the drug with alcohol alone, 25.8% with heroin, and 39.4% with benzodiazepines. Table 1 presents sociodemographic data for the study groups, identifying a significant association between the group and their gender and age. Table 2 shows data on the incidence of HCV infection in the compared patient groups; it is worth noting that there is a statistically significant relationship between the groups described. For example, the group using mephedrone together with alcohol had practically no HCV infection, in contrast to the group using mephedrone and heroin together. And in the group of benzodiazepine addicts, none of the patients were infected with HCV.
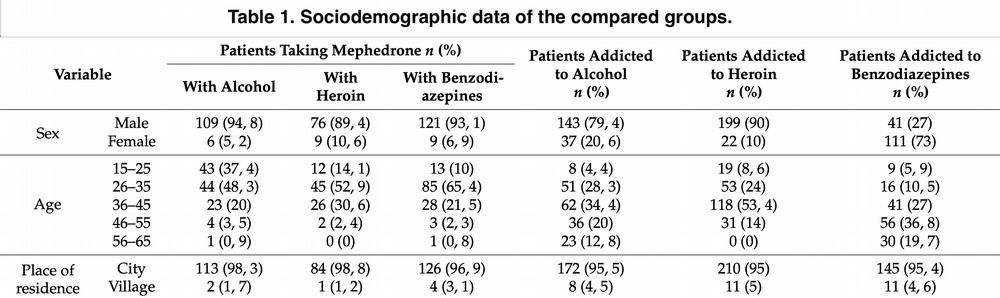
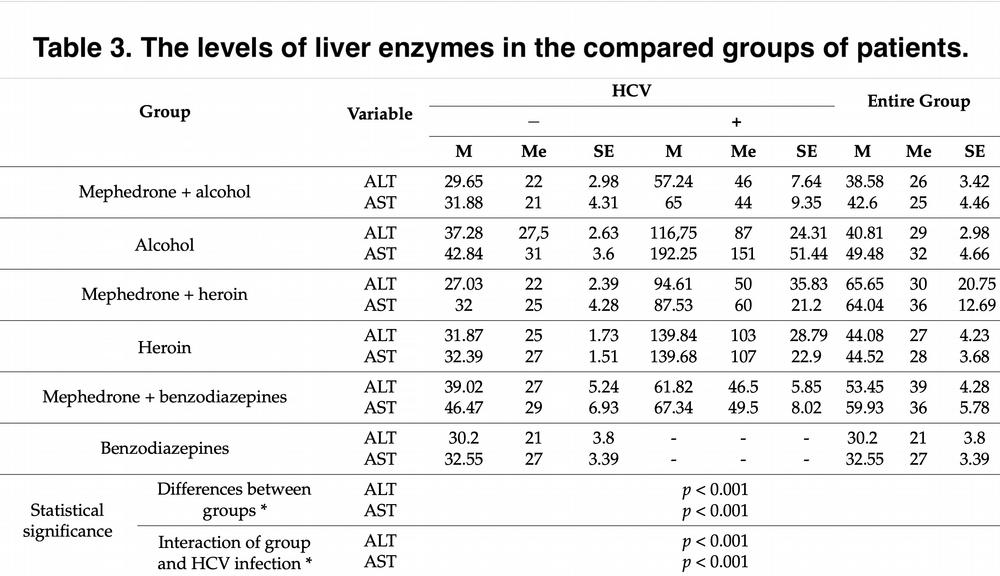
Table 3 shows us descriptive statistics of liver enzyme values. Patients addicted to heroin had significantly lower ALT levels compared to patients who used mephedrone. In the case of alcohol, no statistically significant differences were observed. Similar results are characteristic for AST values.
What is noteworthy is the statistically significant interaction of the group of patients with HCV infection. The obtained results indicated that in the group of patients without HCV infection, there were no statistically significant differences between individual groups of patients in terms of liver enzyme levels. The analysis of simple main effects also showed that in each of the six studied groups of patients there were statistically significant differences between patients infected or not infected with HCV. In individual groups of patients, i.e., infected with HCV, the levels of both enzymes turned out to be statistically significantly higher compared to similar groups of patients without HCV infection.
Those who were infected with HCV and heroin addicts had significantly higher ALT levels compared to those who were infected with hepatitis and used mephedrone in conjunction with heroin. Similar differences were observed in patients who were simply infected with HCV. It is noteworthy that when HCV infection was not taken into consideration, there were no statistically significant differences between patients addicted to alcohol and those who combined alcohol with mephedrone.
In our study, the rate of HCV infection in the heroin-dependent patient group is lower than in the sample study published by Roux (in which the rate is 35%). This may be due to certain factors. For example, the risk of HCV infection is higher in patients combining heroin with alcohol and cocaine, and in our study we studied patients addicted to heroin only. The effects of additional alcohol intake, such as disinhibition, loss of judgment, improved mood or depression may contribute to the involvement of patients in risky sexual behaviour and, consequently, there is an increased likelihood of HCV transmission.
Also, our results show that 61.5% of patients who combine mephedrone with benzodiazepines are infected with HCV. This is probably due to the fact that both benzodiazepines and mephedrone use very much impair cognitive function. This claim is supported, for example, by the Freemen study, which found that cognitive function is significantly impaired in people who use mephedrone compared to a control group of patients. The same is true for patients who use benzodiazepines.
A meta-analysis carried out in 2020 indicated that overuse of benzodiazepines can significantly affect cognitive functions. Cognitive deficits aggravate the difficulty in achieving lasting abstinence. Disturbances of consciousness resulting from the influence of psychoactive substances, aggression, or loss of control over one’s body may expose one to experience unwanted or risky sexual interaction. This may increase the risk of HCV infection. In view of the above, it seems necessary to develop a strategy to prevent benzodiazepine addiction, including patients on mephedrone binge. This could reduce the percentage of patients with HCV infection, and thus the associated morbidity and mortality. The level of information and knowledge about the risk of HCV infection should be much higher among drug users. Social prevention should take place in places frequented by people who use mephedrone and other substances (nightclubs, rave parties, on the street).
Conclusion
As the result of our study showed, high values of liver enzymes were characteristic of all groups additionally infected with HCV. Patient groups without co-infection did not differ in these indices. In addition, the group that was dependent on heroin or benzodiazepine (with simultaneous HCV infection) had statistically significant elevated levels of liver enzymes compared to the group of people who used mephedrone and were infected with HCV. The above result suggests that the significant factor is not mephedrone, but HCV infection itself, which independently influences the elevation of liver enzymes.
The results obtained are confirmed by the literature data showing that HCV infection in the group of patients addicted to alcohol increases the level of liver enzymes to a statistically significant level. Studies conducted in a group of 819 alcohol-dependent patients with co-infection with HCV also seem to indicate the same. Similar data are characteristic for heroin addicted patients. In one of the published articles, the authors pointed to the fact that in the group of heroin-addicted patients, elevated levels of liver enzymes occurred in patients with HCV infection. In the group of injecting drug users with HCV infection, an increased risk of subsequent hospitalizations has been observed. For this reason, as far as possible, education in the medical community should be conducted to minimize the number of HCV infections in the group of patients taking psychoactive substances. Summarizing the above, we can unequivocally state that HCV infection is a statistically significant factor influencing the increased level of liver enzymes in the group of patients taking mephedrone with other psychoactive substances.
