As far back as the 1960s, methadone began to be used in the treatment of opiate addiction as part of maintenance programs. The main goal of this program was harm reduction and prevention of withdrawal symptoms. Primarily, this effect is associated with a weakening of the pronounced cortisol release response, which in turn helps to reduce the likelihood of relapse to uncontrolled use. Taking methadone at least once a day has been shown to reduce relapse rates and facilitate psychological therapy. Also, taking pure methadone as part of programmatic treatment isolates patients from the recreational circle, where it is possible to purchase psychotropic substances containing various undesirable and toxic impurities.
The therapeutic dose of methadone for programmatic treatment ranges from 60 to 120 mg, although physicians’ opinions are still conflicting. Multiple meta-analyses confirm the effectiveness of methadone treatment and also demonstrate a 75% reduction in the risk of death in heroin addicts. In recent years, more and more patients have been hospitalized for the use of psychostimulants, including mephedrone. The proportion of patients using mephedrone is about 90%, and most of them use it in conjunction with other psychoactive substances on a regular basis. Such patient referrals often determine the need for pharmacological correction of the condition using different medications, which increases the likelihood of undesirable drug interactions. In this publication we will tell you about the optimization of the effectiveness of the methadone program we developed in a group of patients who were addicted to mephedrone.
Research design and methodology
101 individuals who used mephedrone together with heroin between 2010 and 2019 took part in the methadone program. Mephedrone and heroin were administered intravenously to all individuals in the study. The methadone program entails giving patients who are unable to stop using the medicine regulated doses of the substance. Patients come to the mental health facility to receive methadone, which replaces the narcotic for them. Qualification requirements for the methadone program were being of legal drinking age, having a heroin addiction diagnosis, and providing the hospital your written approval. In the study group, a maximum of 150 mg of methadone was consumed, with a median dose of 90 mg. A mephedrone binge was characterized as consuming the drug for at least two days. There were 129 people who were dependent on heroin. Patients were routinely checked for their use of psychoactive substances like alcohol and other drugs while enrolled in the methadone program. The fact that individuals violated the methadone program’s restrictions by using substances other than the prescribed methadone was linked to subsequent hospitalizations. Based on a qualitative investigation, urine tests were used to confirm the presence of mephedrone and heroin analytically. Hospitalized patients were the subject of this retrospective investigation. Sex, age, residence, dose of methadone taken, liver enzyme activity, and the number of hospitalizations were among the factors that were gathered.
Results of the study
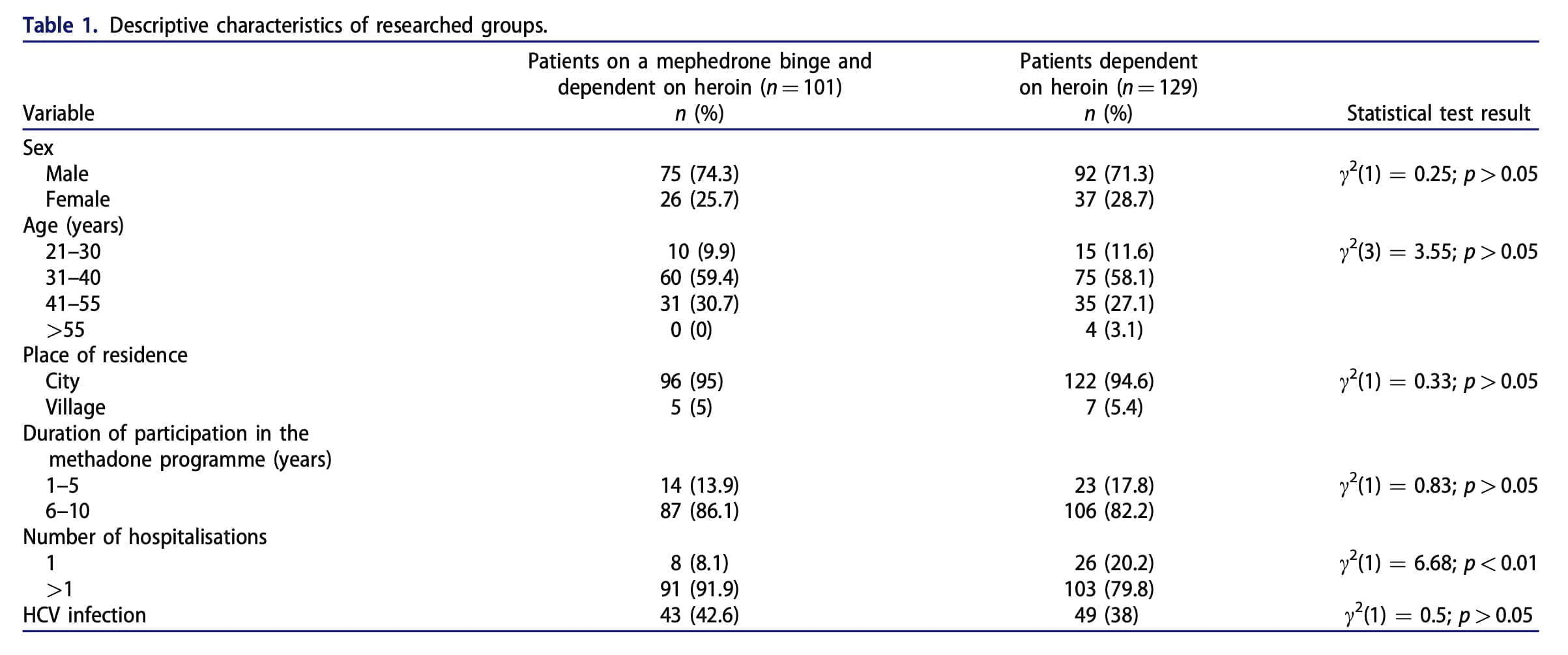
The proportion of male respondents was 74.3%, with the largest group consisting of men between 31 and 40 years of age (Table 1). The average dose of methadone used was about 90 mg. In the group of patients who used mephedrone, HCV infection was detected in 42.6%, and in the group of people who used heroin, this figure was 38%. Patients who were admitted to the hospital due to habitual mephedrone use did not consume the drug by itself; they also took heroin. Most studies in the literature show that people who take new psychoactive substances also take other medications. For this reason, a comparison between two patient groups was conducted: those who were enrolled in the methadone program because they were heroin users, and those who were enrolled because they were mephedrone and heroin users. This made it possible to examine how the methadone program would fare if mephedrone and heroin were consumed together.
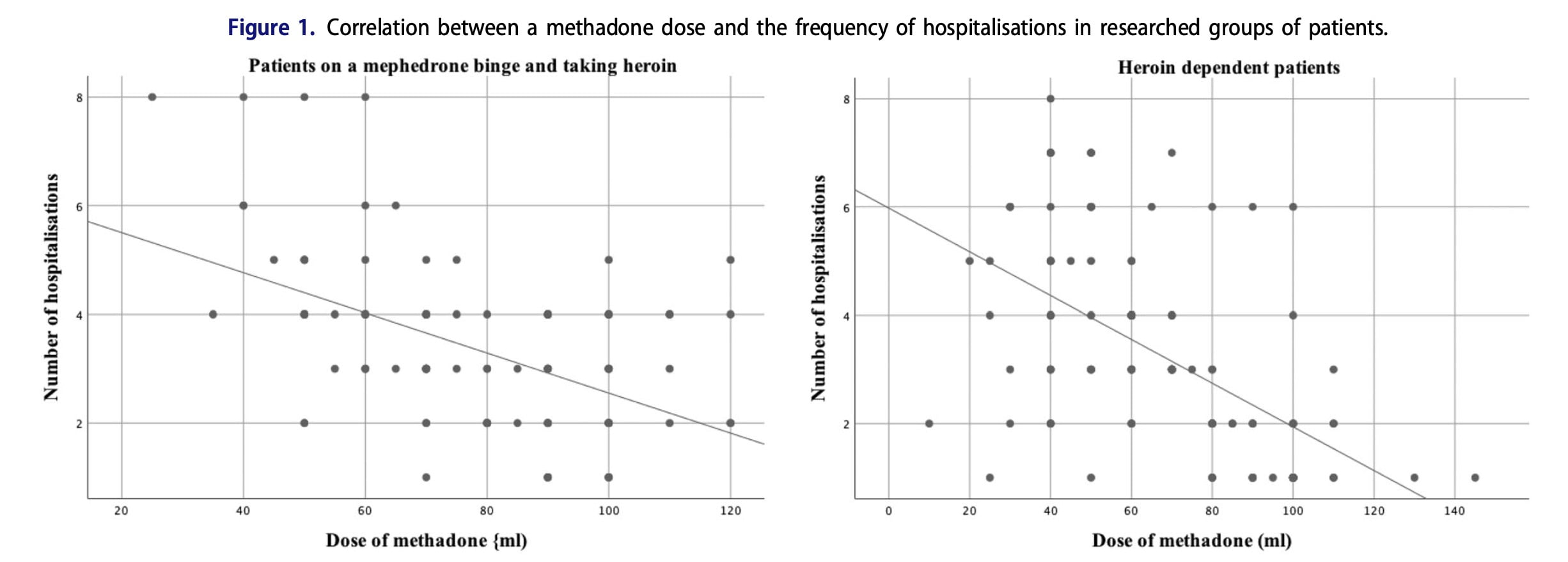
Table 1 demonstrates a statistically significant relationship between the study group and the number of hospitalizations. The most frequent repeated hospitalizations are in patients of the group that are on mephedrone binge. A strong correlation was observed between the methadone dose and the frequency of hospitalisation of a group of people on a mephedrone binge and in a group of people taking heroin. We looked at the liver enzyme activity in the HCV-infected patient group in research groups. When compared to patients who were dependent on heroin, those who had just binged on mephedrone and had HCV infection had much higher liver enzyme activity (Table 2). Therefore, we focused on a group of patients who used mephedrone.
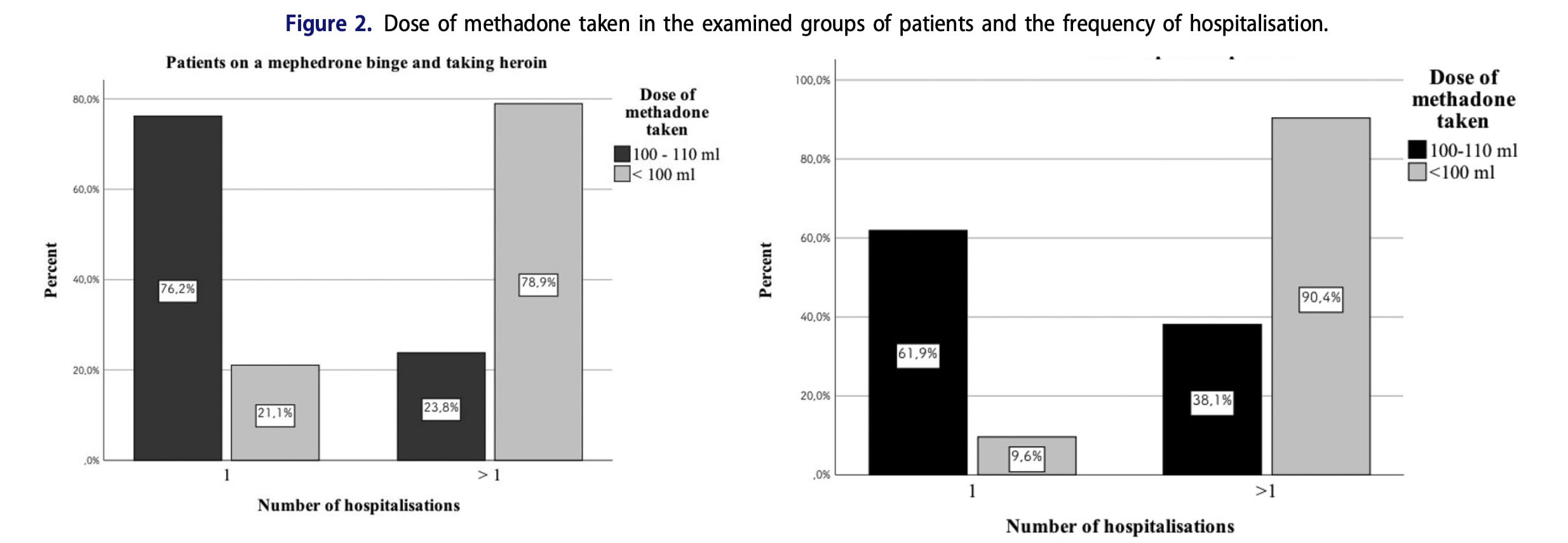
In this study, the effects of treatment duration and methadone dosage in the group of participants who experienced mephedrone binges were examined using the results of moderated regression analysis (Table 3). A significant predictor of the number of hospitalizations is the interaction between the sex of the study subjects and the dose of methadone taken; specifically, it accounts for up to 80.3% of the variance in this dependent variable, while the dose of methadone accounted for just 12%. Similar results apply to HCV infection. The interaction of HCV infection with the dose of methadone taken explains 67.6% of variance in the dependent variable, which is the number of hospitalisations of the subjects. The interaction of three predictors: the dose of methadone, the sex of the subjects and HCV infection explains 48.3% of variance in the number of hospitalisations in the studied group (Table 3).
Methadone generates minimal tolerance and lessens the need to use the drug and the impulse to consume it as it binds to l receptors more tightly. Methadone has been used to treat opioid addiction for more than 40 years, and this experience has shown that it is safe and does not have any negative effects on the body, even when used chronically for a long time. The effectiveness of substitution therapy is demonstrated in a group of patients with opioid dependence and post-traumatic stress disorder. The results obtained in our study are the first data demonstrating that the dose of methadone taken plays an important role in the rate of hospitalizations in mephedrone-dependent patients. The best dose of methadone in a group of people who use mephedrone and heroin together is about 100 mg. In a moderated analysis, we found that patient gender and HCV infection were important criteria for hospitalization frequency. This relationship with the dose of methadone taken explains the obtained 80% of the variance in the frequency of hospitalizations.
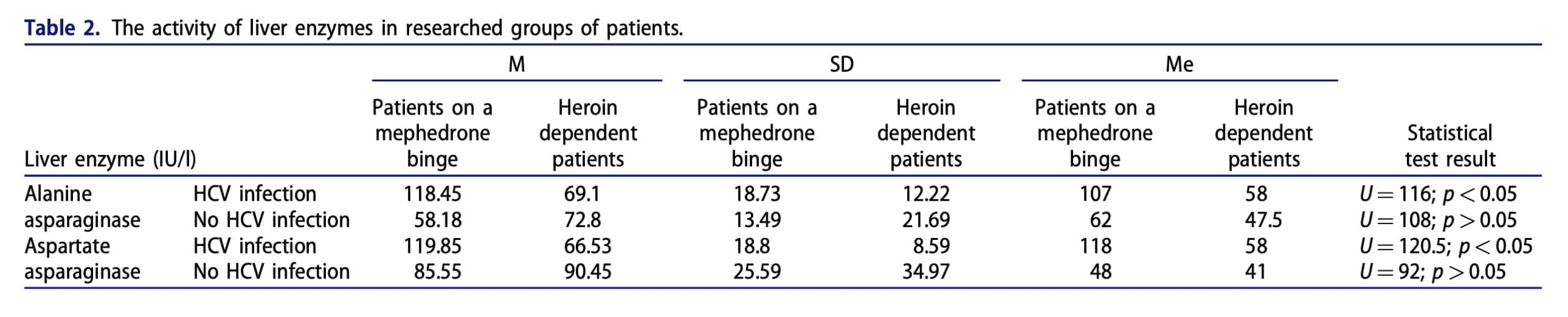
The risk of HCV infection is considerably increased by the use of novel psychoactive drugs, such as mephedrone. According to American statistics, the prevalence of HCV infection among drug users ranges from 63% to 90%, and a cohort study examining the relationship between HCV infection and length of addiction reveals that the risk of HCV infection is 64.7% during the first year of intravenous drug use. As a result, there is a lower likelihood of producing a therapeutic effect and harm to the liver parenchyma. Since methadone is metabolized primarily in the liver, factors like HCV infection and the consumption of other additional psychoactive substances may diminish the therapeutic effect of methadone, which is why liver function should be monitored in order to optimize the treatment of patients addicted to mephedrone.
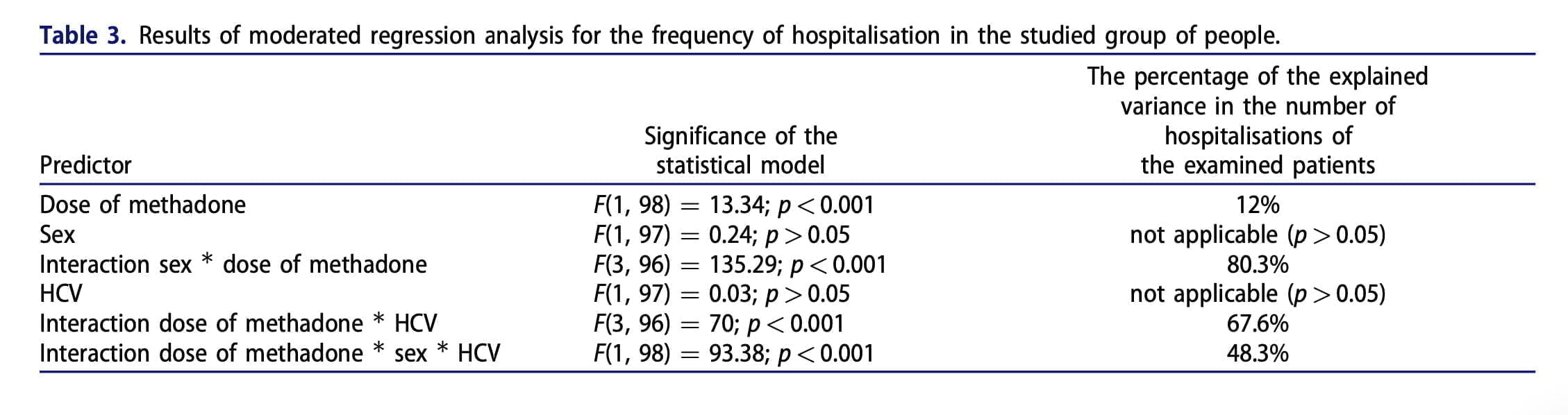
Several factors may be linked to a higher percentage of variation in the frequency of hospitalization in women. Those women who are unemployed or unmarried and young start using heroin earlier than men. Opioids are mainly used by men for leisure. Men experience addiction more slowly than women do. Compared to women, they had less severe psychological and physiological issues during admission. Individual publications address pregnant women when it comes to methadone dosage. In this category of female patients, 60 mg or more of methadone is the recommended dosage. Thus, the results obtained in our study confirm that the dose of methadone taken has a statistically significant correlation with the rate of hospitalization of patients. This applies also to heroin and mephedrone intake together, especially it concerns women and patients who are infected with HCV.
